Buspar Interactions: What Medications to Avoid
Common Drug Classes That Dangerously Interact with Buspar
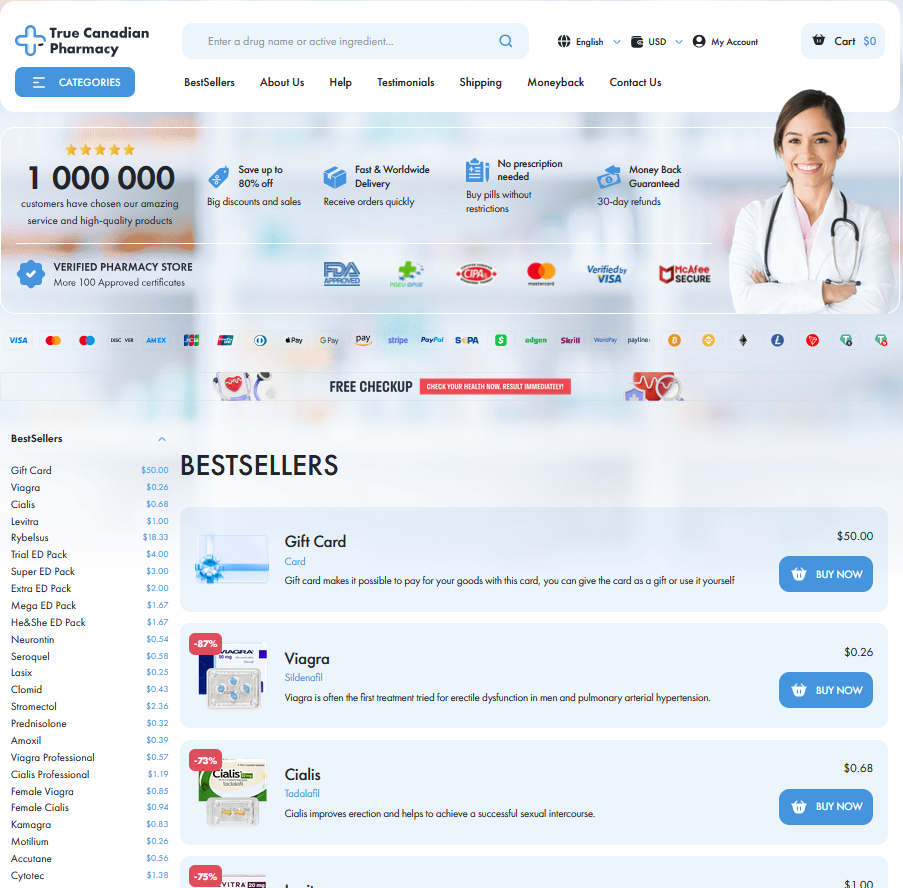
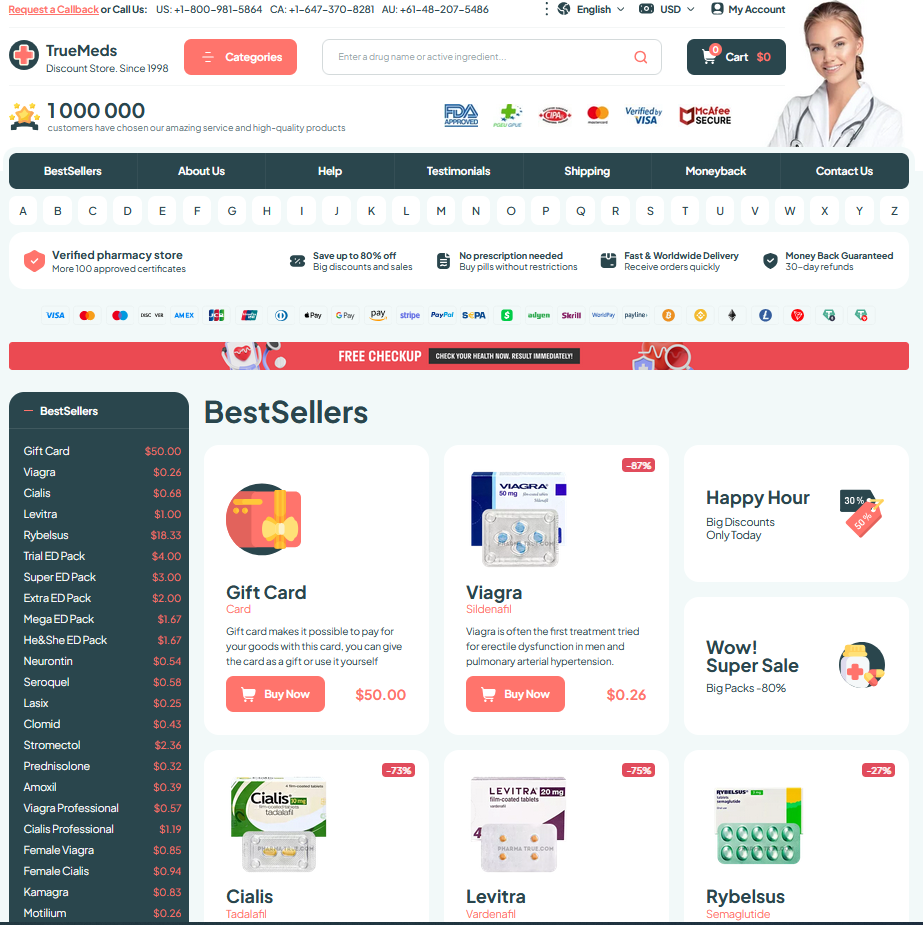
I remember sitting across from a patient who mixed prescriptions without asking; that story sticks because interactions can flip calm anxieties into emergencies. Certain widely used classes—like MAOIs, SSRIs, and some antifungals—change blood levels and brain chemistry in unexpected ways, making vigilance neccessary.
Doctors and pharmacists must talk to patients about opioid sedatives, benzodiazepines, and strong antibiotics; combinations raise drowsiness, serotonin overload, or dangerous cardiac effects. Always check labels, ask about OTC remedies, and avoid improvisation when starting or stopping medicines.
If you take multiple prescriptions or supplements, create a list to share at appointments and use a single pharmacy when possible. Pharmacists can reconcile interactions and recomend safer alternatives or dosage changes; coordinated care lowers risk and keeps therapy effective. Report new symptoms or side effects without delay.
| Class | Risk |
|---|---|
| SSRIs | Serotonin syndrome |
| MAOIs | Hypertensive crisis |
| Benzodiazepines | Excessive sedation |
Antidepressants and Serotonin Risks What to Avoid

Starting buspar while already taking an SSRI or SNRI can feel harmless at first, but it risks raising serotonin to unsafe levels. Doctors worry most about MAOIs or combinations that potentiate serotonin — those mixes can trigger a rapid cascade of symptoms.
Patients should watch for agitation, tremor, rapid heartbeat, fever and confusion; severe cases may include hyperreflexia and seizures. If even mild symptoms occur, seek medical advice immediately to prevent escalation.
Clinicians usually avoid pairing MAOIs with buspar and monitor other antidepressants closely, adjusting doses or choosing alternative therapies. Teh safest plan is clear communication with your prescriber and never stopping medications abruptly without guidance. Bring an updated meds and supplements list to appointments.
Blood Pressure and Heart Medicines Raising Concerns
In clinic scenes, heart drugs alter the story. Patients taking buspar must promptly report beta-blockers, calcium blockers, and antiarrhythmics to their clinician.
CYP3A4 inhibitors such as verapamil or diltiazem can elevate buspar concentrations, increasing dizziness and orthostatic hypotension risk, particularly in elderly patients significantly.
Clinicians should monitor heart rate, blood pressure, and ECG changes. Occassionally dose reductions of buspar or cardiac drug are advised after careful review.
Pharmacists can advise on alternatives and timing; avoid grapefruit with buspar, watch for lightheadedness, and seek urgent care for fainting or palpitations immediately.
Over the Counter Herbal Supplements That Alter Buspar Levels

Imagine reaching for a bottle of calming herbs at the pharmacy; many people assume natural equals safe. For those taking buspar, even supplements can change drug levels or effects.
St. John's wort can markedly lower buspar concentrations by inducing CYP3A4, while 5‑HTP and SAMe may raise serotonin activity, theoretically increasing the risk of adverse effects or serotonin-related symptoms.
Kava and valerian, often used for anxiety or sleep, can amplify drowsiness, dizziness, and cognitive blunting when paired with buspar. Kava also carries liver toxicity concerns, complicating choices seriously.
Occassionally patients omit herbal use from medication lists; ask a pharmacist before mixing remedies with buspar, watch for changes, and consider safer prescription alternatives or adjusted dosing plans.
Recreational Substances and Alcohol Interaction Dangers Explained
Late at night a person reaching for a drink or a pill might not think about buspar, but small choices matter. A social sip can amplify drowsiness and blur judgement, creating a risky begining for anxiety treatment.
Mixing alcohol or sedatives with buspar often increases dizziness, faintness and impairment. Stimulants can produce erratic heart or mental effects. Combining serotonergic party drugs raises theoretical serotonin syndrome risks; be cautious and informed.
A quick reference clarifies common culprits and immediate dangers:
| Substance | Risk |
|---|---|
| Alcohol | Increased sedation and impaired coordination |
| Benzodiazepines | Excessive sedation, respiratory depression |
| MDMA/SSRIs | Serotonin syndrome risk, agitation |
If you or a friend experience worrying symptoms after mixing substances, seek medical help immediately. Tell clinicians about buspar and any recreational drugs. Avoid abrupt stopping; review alternatives with a prescriber who understands your lifestyle and can adjust managment or dosing when needed.
Managing Interactions Monitoring Dosage Adjustments and Alternatives
Begin with a patient who felt sudden dizziness after adding a new prescription. Emphasize early monitoring: prompt checkups, symptom logs, and clear communication so clinicians can be refered to interaction risks before serious effects develop.
Dose adjustments are often gradual, like tuning an instrument: small changes and observation matter. Clinicians may lower or space doses, or choose alternative agents with safer profiles, balancing anxiety control against interaction hazards and tolerance.
Active monitoring includes periodic vital signs, ECG when combining cardiac agents, and lab checks for metabolic interactions. Educate patients on serotonin syndrome signs, excessive drowsiness, and to call promptly if new symptoms occur or worsen.
When interactions are likely, consider alternatives like SSRIs with different profiles, nonpharmacologic therapies, or referral to a clinical pharmacist. Create an emergency plan, document changes, and schedule follow-up to reassess efficacy and safety periodically again. MedlinePlus: Buspirone PubChem: Buspirone